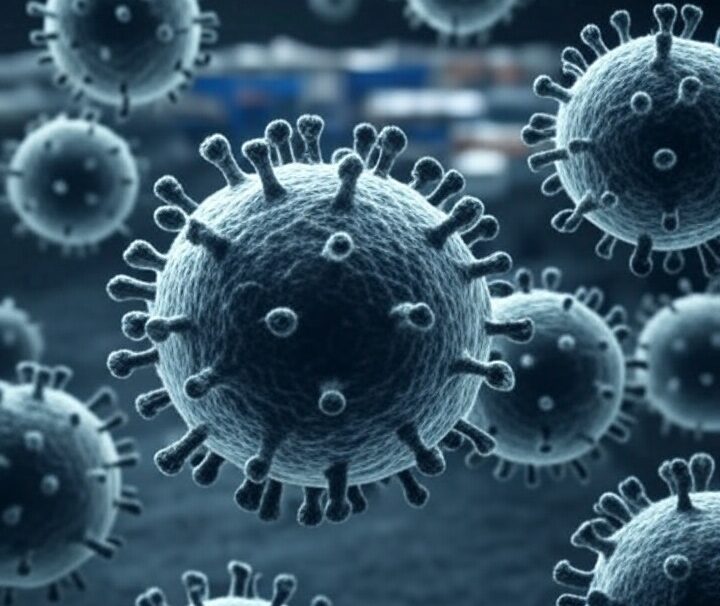
COVID-19, caused by the novel coronavirus SARS-CoV-2, emerged in late 2019 and rapidly transformed into a global pandemic, reshaping societies, economies, and healthcare systems worldwide. First identified in Wuhan, China, the virus spread swiftly, prompting unprecedented public health responses. This article provides a detailed exploration of COVID-19, covering its origins, transmission, symptoms, prevention, treatment, and long-term impacts, while reflecting on lessons learned and ongoing challenges as of May 2025.
Origins and Emergence
SARS-CoV-2, a beta-coronavirus, likely originated in bats, with evidence suggesting a possible intermediate host, such as pangolins, before zoonotic transmission to humans. The first cases were reported in December 2019 at a seafood market in Wuhan. Genetic studies indicate the virus shares 96% similarity with bat coronaviruses, supporting the zoonotic origin hypothesis. Despite extensive investigations, the exact pathway of transmission to humans remains under study, with early debates about natural versus laboratory origins largely resolved in favor of a natural spillover, though some questions persist.
Transmission and Spread
COVID-19 spreads primarily through respiratory droplets and aerosols produced when an infected person coughs, sneezes, talks, or breathes. The virus can also spread via contact with contaminated surfaces, though this is less common. Airborne transmission, particularly in enclosed spaces with poor ventilation, has been a significant driver of outbreaks. The virus’s basic reproduction number (R0) initially ranged from 2 to 3, meaning each infected person could infect 2–3 others, though variants like Delta and Omicron increased transmissibility.
Asymptomatic and presymptomatic transmission complicated early containment efforts, as individuals could spread the virus without showing symptoms. Variants, such as Alpha, Delta, and Omicron, emerged over time, each with distinct mutations affecting transmissibility, severity, or immune evasion. By 2025, subvariants of Omicron have dominated, with ongoing genomic surveillance tracking new mutations.
Symptoms and Clinical Presentation
COVID-19 symptoms vary widely, ranging from asymptomatic cases to severe, life-threatening illness. Common symptoms include:
- Fever or chills
- Cough
- Shortness of breath
- Fatigue
- Muscle or body aches
- Loss of taste or smell
- Sore throat
- Headache
Severe cases can lead to pneumonia, acute respiratory distress syndrome (ARDS), and multi-organ failure, particularly in older adults or those with comorbidities like diabetes, hypertension, or obesity. Long COVID, a condition involving persistent symptoms like fatigue, brain fog, and respiratory issues months after recovery, affects an estimated 10–20% of patients, posing ongoing public health challenges.
Diagnosis and Testing
Diagnosis relies on molecular tests (e.g., RT-PCR) to detect viral RNA, antigen tests for rapid screening, and antibody tests to identify past infections. RT-PCR remains the gold standard due to its high sensitivity. Testing strategies evolved during the pandemic, with mass testing, contact tracing, and wastewater surveillance becoming critical tools for monitoring outbreaks. Home testing kits, widely available by 2025, have empowered individuals to monitor their status, though accuracy varies.
Prevention and Control
Preventing COVID-19 involves a multi-layered approach:
- Vaccination: Vaccines, including mRNA-based (Pfizer-BioNTech, Moderna), viral vector (AstraZeneca, Johnson & Johnson), and protein-based (Novavax) options, have been pivotal in reducing severe outcomes. By 2025, booster shots targeting variants are routine, with annual updates akin to influenza vaccines. Global vaccination coverage, however, remains uneven, with low-income countries lagging.
- Non-Pharmaceutical Interventions (NPIs): Mask-wearing, social distancing, and improved ventilation reduced transmission, especially pre-vaccine. High-quality masks (e.g., N95) remain recommended in high-risk settings.
- Hygiene: Handwashing and surface disinfection curb fomite transmission.
- Public Health Measures: Lockdowns, travel restrictions, and quarantine protocols were widely used early in the pandemic, with varying success. By 2025, targeted measures like localized restrictions during surges are more common.
Treatment and Management
Treatment depends on disease severity:
- Mild Cases: Managed at home with rest, hydration, and over-the-counter medications for symptom relief.
- Moderate to Severe Cases: Hospitalization may involve oxygen therapy, corticosteroids (e.g., dexamethasone), and antivirals like remdesivir or Paxlovid. Monoclonal antibodies, once widely used, have waned in efficacy against newer variants.
- Critical Cases: Intensive care, including mechanical ventilation or extracorporeal membrane oxygenation (ECMO), is needed for severe respiratory failure.
Research into long COVID treatments is ongoing, with rehabilitation programs and anti-inflammatory therapies showing promise. Access to treatments remains a challenge in resource-limited settings.
Global Impact
The pandemic’s toll has been staggering:
- Health: Over 700 million cases and 7 million deaths were reported globally by 2023, per WHO estimates, with underreporting likely. Long COVID continues to strain healthcare systems.
- Economy: Global GDP contracted by 3.5% in 2020, with sectors like tourism and retail hit hardest. Supply chain disruptions and inflation lingered into 2025.
- Society: School closures, remote work, and mental health challenges reshaped daily life. Social inequities, including disparities in healthcare access and vaccine distribution, were exposed and exacerbated.
- Science and Technology: The pandemic accelerated innovations in telemedicine, vaccine development, and genomic surveillance, but also fueled misinformation, complicating public health messaging.
Lessons Learned and Future Preparedness
The COVID-19 pandemic highlighted strengths and weaknesses in global health systems. Key lessons include:
- Rapid Response: Early detection and transparent communication are critical to containing outbreaks.
- Equity: Addressing disparities in healthcare and vaccine access is essential for global resilience.
- Surveillance: Investments in genomic sequencing and real-time data sharing can track and mitigate emerging threats.
- Public Trust: Combating misinformation through clear, evidence-based communication is vital.
By 2025, global health organizations have strengthened pandemic preparedness frameworks, including the WHO’s Pandemic Treaty, aimed at improving international coordination. However, challenges like vaccine hesitancy and geopolitical tensions continue to hinder progress.
Current Status and Outlook
As of May 2025, COVID-19 is no longer a global health emergency but remains a persistent threat, with seasonal surges akin to influenza. Vaccination and hybrid immunity (from infection and vaccination) have reduced mortality, but vulnerable populations require ongoing protection. Research continues into next-generation vaccines, universal coronavirus vaccines, and long COVID therapies. Climate change and habitat encroachment raise concerns about future zoonotic pandemics, underscoring the need for proactive measures.
Conclusion
COVID-19 has left an indelible mark on the world, exposing vulnerabilities and driving innovation. While significant progress has been made in managing the virus, its legacy endures in ongoing health, economic, and social challenges. By learning from the past and investing in preparedness, humanity can better navigate future pandemics. Staying informed, vaccinated, and vigilant remains crucial as we coexist with SARS-CoV-2 in an ever-evolving global landscape.











Leave a Reply